Haywood Hospital, Stoke-on-Trent
Introduction
I was admitted to the Haywood hospital on 26th September, 2015; it has a special place in my heart – it’s where my life restarted, or indeed I was reborn.
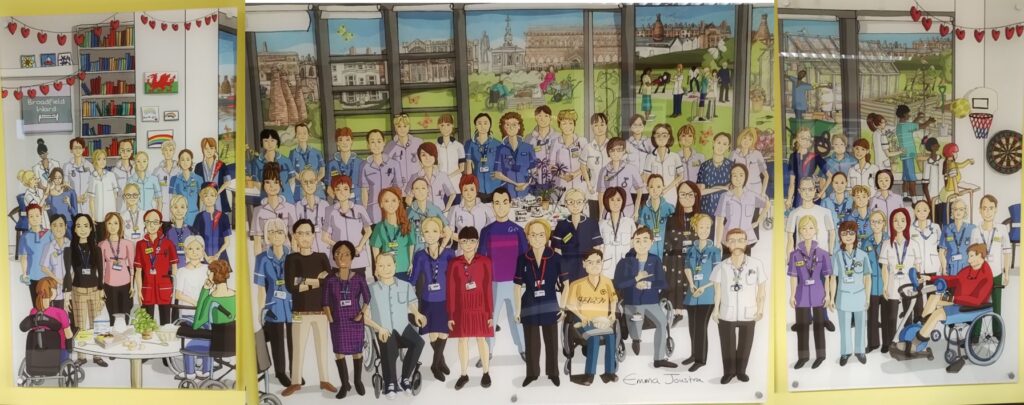
I can summarise my rehabilitation experience on the Broadfield ward of the Haywood hospital in one sentence: “I was admitted as a shell of a person, then discharged home just six weeks later as David Wozny.”
Clicking this link redirects to my Broadfield ward volunteering page, where I commenced a befriending role in 2024.
Clinical Psychology Assessment
The following content was snipped from a clinical psychologist’s report, which was undertaken in November 2015 during my discharge from the Broadfield ward.
Presentation During Assessment
David has displayed a high level of engagement with staff from all disciplines during the assessment period. David is able to understand and comply well with task instructions and has maintained a good level of effort during all of the assessments. David has shown a high degree of self-motivation and appears to enjoy challenges presented to him. During these, he would verbalise sound problem-solving strategies used, which reflected good deductive reasoning. This solution-focussed and determined approach appears consistent with his premorbid personality. David is self-employed as an IT consultant and achieved a first in his degree in engineering. David’s partner, Ruth, confirmed that she has observed no noticeable personality changes in David.
Neuropsychological Status Tests
The following tests were carried out:
- Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)
- Test of Premorbid Functioning (ToPF)
- Neurobehavioural Functioning Inventory (NFI)
- Frontal Systems Behavioural Scale (FrSBSe)
- Hospital Anxiety and Depression Scale (HADS)
Classification scale for the areas tested:
- Very superior
- Superior
- High average
- Average
- Low average
- Borderline
- Extremely low
David scored within the borderline range for immediate memory and language, whilst his scores for delayed memory fall with the extremely low range. This suggests that David’s brain injury has likely affected his cognitive functioning, particularly in relation to these three areas, especially so for delayed memory. Whilst David has reported that he has always had a poor memory, even prior to the injury, the estimation of his premorbid functioning would predict higher levels than that which were recorded. Further analysis of the subtests for the delayed memory domain suggest that David has a particular difficulty with long-term verbal memory encoding and retrieval – that is a high rate of forgetting information he has heard, but a better chance of recalling information that is presented visually.
Summary of cognitive tests indicating strong deficiencies:
- Delayed memory – extremely low (measures delayed recall and recognition for verbal and visual information)
- Immediate memory – borderline (measures initial encoding and learning of verbal information)
- Language – borderline (measures expressive language, fluent use of language)
David’s visuospatial / constructional abilities appear to remain a significant area of strength for him. It bodes well that David has these strong areas, which can be drawn on in his rehabilitation. It is also important to note that David is very early in his journey of recovery and has shown remarkable improvements in his stay here on the ward. It is likely that he will continue to improve with time, more specifically over the coming months.
Mood
In addition to the cognitive assessments completed, a mood assessment was carried out using the Hospital Anxiety and Depression Scale (HADS). David reported no clinically significant problems with anxiety or low mood. This is consistent with the cheery mood with which he has presented himself whilst on the ward.
Conclusion
David has fully engaged in his rehabilitation and has shown a real commitment to remaining goal focussed while transitioning through his post brain injury recovery. The progress David has made during his stay here on the ward is remarkable, and it has been a privilege and a pleasure to witness this. We wish David all the best for the future.
Selfie Photos


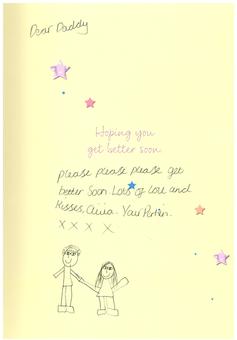
Card from my Daughter
I still treasure the card my then ten year old daughter gave to me when she visited for the first time. Olivia had been deliberately held back from visiting me for the eight weeks while I was in critical care, followed by two weeks on a neurosurgery ward. It was (I consider rightly) felt that if I hadn’t survived, my family didn’t want her last memories of me to have been in my vastly diminished and confused state.
My Experiences of the Broadfield Ward
Much of what I’ve written below, sprung to mind during early 2016 post-discharge reflections on my Broadfield ward experience; there was a little fogginess / lack of clarity in my musings.
- The Haywood Hospital was fabulous. The staff were great, the rooms / wards were comfortable, and the food was fine.
- The term recovery was confusing for me, I wrongly interpreted recovery as meant returning to how I was prior to my injury. Having some modest expectations aligned to the term recovery might have helped me feel like I was making progress.
- I could become a little frustrated when asked to explain how my brain felt; I often used the term cloudy, but nothing could describe the reality. I have now regained a reasonably healthy command of vocabulary and I can still recall some thoughts which crossed my mind, but I’m at a loss to begin describing how it felt. I believe it’s one of those matters which has to be experienced to be properly understood, and it’s not a journey anyone takes by choice.
- Some great advice I received from a psychologist was to stop my habit of short-term memory self-testing. Until I heard these words I couldn’t stop myself, as I’d thought it was a useful practice; however, it had been entirely counter-productive.
- I was initially a little disappointed to be moved from my single room onto a ward. With hindsight, it was a little bit closer to the normality of dealing with people, such as patients with TVs being too loud or swearing endlessly.
- Measuring my recovery progress appeared to me to be arbitrary, and I struggled accepting the psychological tests which were undertaken. I knew I was going to be rubbish at any short-term memory scrutiny because I didn’t have access to any of my coping strategies. Knowing that I wouldn’t have these tools available made me frustrated and more likely to perform poorly. I’ve realised that I don’t like to fail – at anything! I may have benefited from being told that the inaccessibility of coping strategies was deliberate.
- I wasn’t prepared for the outside world upon hospital discharge, despite getting much great advice from the wonderful Haywood staff on this matter. It simply couldn’t sink in that the hospital discharge stage was only a step on my recovery journey. Ruth spending a night by my bedside at the Haywood might have helped her understand where my head was at, as there must only have been so much Ruth could have understood from her two-hour visits.
- I hadn’t realised how much apologising I was doing for memory related matters; I found it very difficult to stop myself, but I needed to be told (by Ruth).
- I couldn’t figure out / comprehend the numerous staff roles, e.g. neuro-x / psychiatrist / psychologist; it was bewildering. Further to my discharge, I still became frustrated when arranging follow-up appointments and being asked if I was referred by neuro or psych, etc. I don’t know how this matter can be improved though; a printed handbook would hardly be a solution. I knew this was necessary for clinical professional purposes, but as a patient I felt I needed to comprehend these different terms / roles so that I could understand who was doing what with me. In correspondence I saw job titles such as “Clinical Psychologist – Neurorehabilitation”, it was frustrating for me at the time.
- It’s similar with the names for the University Hospital North Midlands or the Royal Stoke Hospital or the City General – it always ended up being “the hospital near to Newcastle.” I imagine it may be understood by the clinical professionals, but for myself (and my mother), it was an area of misunderstanding.
- More appointments with rehabilitation consultants would have been helpful in steering me on my recovery journey, and giving me practical advice. There needed to be three of Dr Alex Ball – she was special. 🙂
My Broadfield Ward Diary Entries
I kept a daily diary during my recovery period on the Broadfield ward; I’ve transcribed the entries below.
Friday 2nd October 2015
Ruth was here at 09:00 on a Friday, she caught the end of occupational therapist tests for standing, walking, turning, etc. We went over to Hartshill for eye tests in an ambulance just after nine. I felt I did everything satisfactorily, the tests finished at about 10:45, I then had an appointment with Ruth regarding my planning back at main ‘Heathfield’ centre. [DMW: I recalled the hospital name Haywood incorrectly] There was a cock-up with the ambulances, so we ended up not getting back until 15:00. A long wait for me, but must have been incredibly tedious for Ruth.
When we did eventually arrive, Les Phillips was in Heathfield reception, so it was lovely to catch up with him. Ruth was very patient and pleasant throughout and really lovely – digging a deep hole in my heart.
Later on Olivia came, as well as Charlie. They were both on good form so it felt like a lovely family experience. I should count my lucky stars.
Saturday 3rd October 2015
Was raised at 08:00 for toilet, bathing, cleaning, etc. which was excellent. Feel like I’m gonna do my exercises and my Lego and enjoy Saturday for a change. Had a full wet shave from a member of staff which was great. Phoned Sue at 10:00 and we had a lovely catch up.
Done half the Star Wars Lego, but have got stuck doing the assembly *Finished it.
It was lovely to see Mick and Val about 15:00, they were very kind and interested. Ruth came at 18:30 and we had a really lovely evening. She bought some essentials like mouthwash and bodywash which were very welcome. But mainly it just felt lovely chatting to each other – an area in which I feel I have improved this last week. Ruth left after ninety odd minutes – wow – gorgeous face and body – I’m mad about her!
Sunday 4th October 2015
Up at 07:00 for a sit down shower, which was very welcome. I feel clean and refreshed right now (at 08:00). I’ve washed everywhere and shampoo’d twice and scrubbed clean – ace. Had a porridge breakfast in the day room, still no conversation to be had. I had a toilet session in the bathroom and felt much healthier. Update: after my shower I was measured as low body temp and given a blanket. In truth, my fingers and toes were freezing, and I did all sorts to warm them up. By mealtime and a toilet break they were much better. I have taken direction in how to put foot plates on wheelchair – yes! Time of this paragraph 10:15.
Made the rabbit Lego in the day room, it took an hour and my fingers are exhausted.
I got rather tired at about 12:00 and really fancied a lie down. I had a second lunch of cauliflower cheese, but had a coughing fit after eating too much black pepper.
I slept really well with no painkillers and felt knackered getting myself up at eight – no complaints though.
Monday 5th October 2015
I dragged myself out of bed at eight and had a lovely big helping of porridge. Therapists had two physical assistants take me through a wide range of leg and arm movements which was very satisfying. I pushed quite hard, and it was very tiring in the body.
Long morning in my chair – I tried and failed to get the Nationwide App on my iPad working. I am planned to do a walk this afternoon with physical therapists, but apart from that it could be a bit slow.
I had a chicken lunch, then seconds of a vegetable tikka – which seemed so much stronger than everything else I have had, but was very nice nevertheless, and no problems with coughing or anything.
I spent the afternoon lying in bed. Later on I did those walking sessions which went very well just outside my room, staff were positive and so was I. Blood pressure was measured as 94, which is a bit low apparently – but nothing to worry about. I saw Ruth at 18:15 and we had a lovely time, she’s so special. I am lucky to have her.
Slept through to 08:00, very well, just a cough – managed 05:00 wee break to mix in.
Tuesday 6th October 2015
Up at 08:00 in good order and a toilet break. All is well and I feel great. Blood pressure was measured at 108 – though this is straight after my porridge breakfast, I don’t know if that makes a change! Might be a quiet day today as I need to get some recording and video ready on the iPad.
I did my physio exercise during the day around 14:00, it was limited to just abs mainly, but I became knackered. I slept on the bed for two hours. Tea was a fish concoction that was puree rather than pre-mash – I asked for the latter – but no chance!
It’s now 18:10 and I’m just waiting for Ruth and mum to arrive which is very exciting. I feel that I’m becoming more self-sufficient, and when I get a bit more strength / co-ordination / brain ability, I’ll be a more useful person.
Changes in staff are a little weary. I think the physio girl who was good had left for another job, and the occupational therapy lady is off long-term sick with her child. The shoulder bloke is weirding me a bit. Karen is definitely the star assistant – always a good help.
Wednesday 7th October 2015
Nice self-get up at about 08:00. I did mentality and eating tests – mentally good, though recognised the risk of not having thickened juice after a coughing fit. With speech language and swallowing team. Did some painting but then got a long back pain. Moved onto my physical health team and did walks, lunges, twists, etc. It went reasonably well, though the legs do tire very quickly. I had a towel fitted to my wheelchair to try to reduce instances of back pain.
Thursday 8th October 2015
Full, busy day with lots of physical exertion – very good.
Ruth came about 18:30 and it was lovely.
I did FaceTime with Olivia for an hour later, she showed me her new dressing table / chest of drawers.
Friday 9th October 2015
Up at 07:30 by Russian lady for a very severe clean and preparation for the next task. Did porridge breakfast for myself in the kitchen, which felt good to be doing a real task. I tidied the room up and I am rather tired, I think this afternoon I’ll do a bit of leg exercises then shut eye until Olivia comes about 18:00.
I had a lovely afternoon with Ruth where she was a bit fed up with work, but planning a nice, simple evening. Olivia arrived about 17:30 and it was lovely, just having proper, intimate conversation without her having any other distractions. She was very open and engaging, it was a delight.
Saturday 10th October 2015
Good sleep, better porridge (less thick than mine). Had a birthday call from Sue / Keith (sister / brother-in law) which was lovely, then a birthday call with Laura (niece) which was fabulous. I learned about her plans for Thailand, Brazil (Amazon River) and then Canada – probably happening in April 2016. She’s very confident that she can get work again when she comes back – and so she should be. I did putty exercises in the morning and gave myself a good clean up.
Thursday 29th October 2015 – Recap in August 2017
A colleague of mine from my place of employment at the time of my injury (London’s Met Police) visited me. I was an IT security consultant and Phil Dear came to see how well my recovery was going as I was deeply involved in some important work for the Met. I’d last met with Phil on 16th July 2015 in London. I thought I was recovering really well and might be available to return to work for the Met in a couple or three months. Little did I know that it would be two years after my injury before I set foot in professional employment, back with the Met in July 2017.